Musculoskeletal (MSK) Research
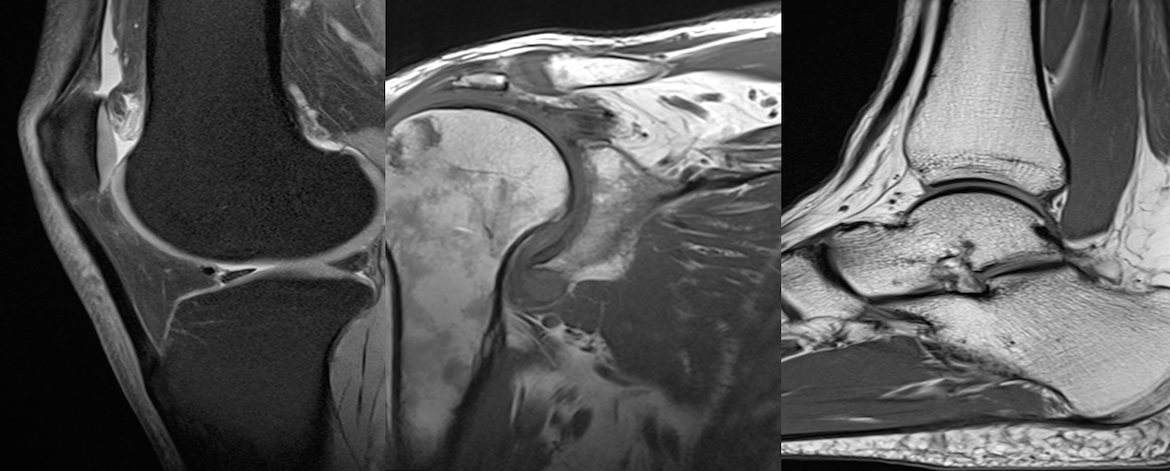
Here at CFMM, On the 3 Tesla magnet. We have a number of muscularskeletal studies. These include Ankle, knee and shoulder imaging. With all of Siemens specialty coils availabile and a wide variety of pulse sequences the following studies use to collect their data.
A Randomized Trial of High Tibial Osteotomy
PI: DR Trevor Birmingham
Department: Physical Therapy
Award Value: Reduced scanning rate
IMPACT: Knee osteoarthritis (OA) is a leading and growing cause of pain and disability worldwide. There are currently no treatments shown to alter OA progression in humans. High Tibial Osteotomy (HTO) is a limb re-alignment surgery intended to correct aberrant knee (tibiofemoral) joint loading in patients with early knee OA, thereby slowing, halting or even reversing degeneration of articular cartilage. We are conducting a randomized trial comparing patients with and without undergoing HTO. Outcomes are changes in MRI measures of articular cartilage morphology; biological markers from synovial fluid, serum, and urine; biomechanical measures from 3D gait analysis; patient-reported outcomes; and costs - assessed at baseline, 12 and 24 months. We hypothesize that results will demonstrate, for the first time, that a biomechanical intervention (HTO) can slow disease progression and improve quality of life. Additionally, the combination of measures will provide a rich source of data that will enable us to answer several clinical and basic science questions related to OA progression that are imperative for the advancement of treatments.
We plan to test the hypothesis that, through the application of a standardized and functional loading stimulus, abnormal qMRI findings that are evident in knee articular cartilage of individuals with OA can be evoked in individuals at risk for knee OA. Further, we will test the hypothesis that limb realignment surgery, intended to improve medial tibiofemoral joint cartilage function, will improve the qMRI measures observed preoperatively. We will use a standardized loading stimulus enabled by a state-of-the-art treadmill, capable of moving with 6 degrees of freedom, that challenges the knee in a functional manner, and that can be repeated exactly at a later time. We plan to use the Siemens 3 Tesla Magnetom Prisma at the CFMM to assess qMRI measures immediately before and after (within 10 min) the loading stimulus. Given the exploratory nature of this investigation, we plan to begin testing with 10 young healthy subjects without knee pathology, 10 patients at risk for knee OA (ie. varus aligned limb with previous ACL injury but with minimal-to-no joint space narrowing), and 10 patients with established, isolated medial knee OA (joint space narrowing) undergoing limb realignment surgery, and repeat the tests on those same 10 patients 1 year after surgery. With scans completed pre (1hr duration) and post (30 min duration) the loading stimulus, 80 testing sessions x 1.5 hrs = 120 hours of scan time are requested. If provided the reduced rate, we currently have funds from two internal research grants to carry out this preliminary work – that we suggest is essential for succes with future external grants.
Acute Achilles Rupture
PI: DR Trevor Birmingham
Department: Physical Therapy
Award Value: Reduced Scanning Rate
The Achilles is the thickest and strongest tendon in the human body. However, it is the most commonly ruptured tendon in the adult population and it’s incidence has risen exponentially over the the last decade. While acute Achilles tendon ruptures (AATRs) can be treated surgically or conservatively, previous randomized trials suggest no benefit of operative versus non-operative treatment with functional rehabilitation. Despite these findings, surgery is very frequently performed with the rationale that operative care results in superior long-term outcomes for tendon structure and therefore, functional activities. However, since the long-term physiological and pathological changes associated with AATR healing are not well understood, this claim lacks evidence. Previous work at the Fowler Kennedy Sports Medicine Clinic (FKSMC) followed non-operatively treated AATR patients with serial MR images at 6, 12, and 24 weeks post-injury. It was found that imaging abnormalities persisted at 24 weeks, so the authors suggested longer-term MRI evaluation would be beneficial to define an end point of healing after an AATR. In addition, the authors suggested future studies should correlate MR findings with clinical measures. Also at FKSMC, Willits et al. (2010) randomized AATR patients to receive surgical repair and accelerated functional rehabilitation or accelerated functional rehabilitation alone. With the support of staff from the FKSMC and the Wolf Orthopaedic Biomechanics Laboratory (WOBL), we plan to re-recruit patients from the Willits et al. 2010 study to compare long-term structural, functional, clinical and patient-reported outcomes of these previously randomized patients who are more than ten years post-treatment. This study will offer the opportunity to compare both between treatment groups and the affected/ non-affected limb, in up to 80 patients who were previously randomized to treatmemt.
We request the use the 3 Tesla Magnetom Prisma at the CFMM at the reduced rate to evaluate tendon healing in patients who are greater than;10 years post-treatment. Based on previous work, we plan to evalute Achilles tendon length, cross sectional area at the calf, diameter of the tendon at the tear site, gastrocnemius signal intensity, background tendon quality and the presence of a gap in the tendon. We also plan to correlate MRI findings with functional, clinical and patient-reported outcomes. The ability to investigate advanced measures of tendon integrity in this unique group of AATR patients previously randomized to treatment will provide the best evidence to date about the optimal treatment for this very common and serious injury
Evaluate the healing rates of posterior meniscus root tears 12 months post-surgery
PI: DR Alan Getgood
Department: Physical Therapy
Award Value: Reduced Scanning Rate
The meniscal posterior roots not only provide a chondroprotective function to the knee, but also aid in providing anteroposterior and rotatory stability. Repair of root tears has become common clinical practice, however there is currently a lack of research investigating meniscal healing rates following posterior root repair. Furthermore, it is unclear whether the the repair and subsquent healing will confer greater stability to the knee when performed in conjunction with anterior cruciate ligament reconstruction. This is a sub-study from our Internaltional Multicenter Randomized Clinical Trial comparing Anterior Cruciate Ligament Reconstruction With and Without Lateral Extra-articular Tenodesis in Individuals Who Are At High Risk of Graft Failure. A number of pateints were prospectively identified as having root tears which were fixed. The aim of this study is to correlate healing rates with stability, functional and pateint reported outcome data.
This study will have a impact on when and how the international surgical community should address this type of mensical tear, and could result in direct patient benefits.
qMRI Cartilage Response to Functional Loading Stimulus
PI: DR Trevor Birmingham
Department: Physical Therapy
Award Value: Reduced Scanning Rate
Knee osteoarthritis (OA) is a chronic, progressive condition that places tremendous burden on individuals and societies. The hallmark of the disease is slow, variable degeneration of articular cartilage. Although several factors are likely involved in the etiology of knee OA, aberrant loading of the joint (for example by acute trauma, or by mal-alignment of the limb) is considered a strong risk factor for OA development and progression. One of the major challenges in studying and treating OA is that most methods of detecting cartilage degeneration rely on joint space narrowing identified on x-rays, yet the disease process is well underway by the time such radiographic changes are evident. Recent advances in MRI measures of knee (tibiofemoral) articular cartilage, and their use in large-scale longitudinal studies, demonstrate that relatively subtle changes in disease progression can now be measured. However, the time required to observe such changes is typically at least 12-18 months in patients with established OA, and longer in individuals at risk for OA development. These MRI variables include measures of cartilage morphology, such as thickness and volume, and articular cartilage function quantified as T1rho and T2 relaxation times that detect compromised integrity of the cartilage structure and biochemistry. Quantitative MRI (qMRI) measures show particular promise for earlier detection of OA, prior to radiographic changes. If “harnessed” properly, such measures could have major impact on the field by serving as a marker of early OA disease progression, and provide a way of evaluating potential preventative and/or disease modifying interventions.
We plan to test the hypothesis that, through the application of a standardized and functional loading stimulus, abnormal qMRI findings that are evident in knee articular cartilage of individuals with OA can be evoked in individuals at risk for knee OA. Further, we will test the hypothesis that limb realignment surgery, intended to improve medial tibiofemoral joint cartilage function, will improve the qMRI measures observed preoperatively. We will use a standardized loading stimulus enabled by a state-of-the-art treadmill, capable of moving with 6 degrees of freedom, that challenges the knee in a functional manner, and that can be repeated exactly at a later time. We plan to use the Siemens 3 Tesla Magnetom Prisma at the CFMM to assess qMRI measures immediately before and after (within 10 min) the loading stimulus. Given the exploratory nature of this investigation, we plan to begin testing with 10 young healthy subjects without knee pathology, 10 patients at risk for knee OA (ie. varus aligned limb with previous ACL injury but with minimal-to-no joint space narrowing), and 10 patients with established, isolated medial knee OA (joint space narrowing) undergoing limb realignment surgery, and repeat the tests on those same 10 patients 1 year after surgery. With scans completed pre (1hr duration) and post (30 min duration) the loading stimulus, 80 testing sessions x 1.5 hrs = 120 hours of scan time are requested. If provided the reduced rate, we currently have funds from two internal research grants to carry out this preliminary work – that we suggest is essential for success with future external grants.
Hip Scope vs THA RCT
PI: DR Ryan Degen
Department: Physical Therapy
Award Value: Reduced Scanning Rate
Background and Rationale: Intra-articular hip pathology is a common cause of pain and disability. It often affects working age adults, commonly between the ages of 40-60 years, and is associated with significant productivity losses. Often, these patients are evaluated with radiographs and advanced imaging, such as a magnetic resonance image (MRI), leading to the diagnosis of labral tears, hip impingement and varying degrees of osteoarthritis. Historically, these diagnoses represented challenging entities to treat in this demographic, as minimally invasive treatment options were not readily available. Total hip replacement (THR), which is an irreversible procedure that replaces the diseased joint with a prosthetic, was often not considered in this population, as it was seen as too aggressive for early joint degeneration. Instead, it was conventionally reserved for older patients (average age 69±10 years) with more severe disease. Additionally, there were concerns related to increased physical demands in these younger patients and the implications of this on implant longevity. As a result, these patients were often managed with prolonged courses of non-operative treatment to manage pain and symptoms until disease progression warranted a THR. More recently, advancements in THA have resulted in improved implant designs and novel surgical approaches to enable accelerated recovery, greater postoperative activity levels and increased survival of the joint, thus preventing or delaying the need for revision surgery. These recent innovations in THA, and the lack of compelling evidence to support arthroscopy in this population, question conventional wisdom of reserving THA for end-stage disease. Simultaneously with the improvements in THA, hip arthroscopy has grown in popularity. Arthroscopy is a minimally-invasive, joint-preserving procedure which has seen a tremendous increase in utilization, particularly in the US. This is likely due to advancements in available equipment and surgical techniques. Initially it was seen as a viable option for patients with mild osteoarthritis, for whom a THA was felt to be too extreme. Arthroscopy will be used to perform a labral repair or debridement, and debride or decompress any impingement lesions. Debridement of loose chondral flaps of the joint surfaces may also be performed. However, there is a lack of high-quality evidence to support its effectiveness for patients in this middle-aged demographic. Several small cohort series, have evaluated outcomes following arthroscopy in patients over the age of 40 with rather unimpressive results. They report a relatively high early failure rate among these patients, defined as either a lack of improvement of patient reported outcome measures or failure with conversion to THR within 2 years of their arthroscopy. In several series, the rate of conversion to THR within two years approached 20%. Most poor results are attributed to the presence of concomitant osteoarthritis. However, the majority of these reports on the outcomes and survivorship of arthroscopy in this patient demographic are of limited quality, reported as retrospective, single-institution cohort series. Presently, there is a lack of high quality evidence to guide the treatment of 40-60 y.o. patients with mild to moderate hip OA. Therefore, the aim of the proposed study is to perform a comparative pilot, randomized controlled trial of arthroscopy versus definitive THR for the treatment of mild-moderate hip OA in patients between the ages of 40-60 years. 160 pts (80 in each arm).
All arthroscopy patients will undergo pre-operative and 1 year post-operative magnetic resonance imaging (MRI), to enable quantification of morphological features of the hip joint and chondral degeneration. Plan for Analysis with the plan to publish in a high impact journal: We will conduct a cost-effectiveness analysis from a healthcare payer and societal perspective. We will calculate the incremental cost-effectiveness ratio (ICER) and estimate cost-effectiveness using the net benefit regression framework. We will include baseline HOOS score, age, sex, and BMI as covariates in our regression models. To characterize the statistical uncertainty around our estimate we will calculate 95% confidence intervals, and a cost-effectiveness acceptability curve (CEAC). Important for estimating the long-term outcomes, we will estimate the cost-effectiveness of THA compared to hip arthroscopy over the lifetime of a hypothetical cohort of patients with mild to moderate hip OA using a Markov model. We will parameterize the model using prospectively collected data from the trial, and obtain estimates of failure rates, healthcare resource use, quality of life, costs and clinical outcomes from our institutional patient registry data, administrative datasets and the existing medical literature. Limited funding as been obtained through AMOSO to conduct the Research MRIs. The reduced rate will allow us to conduct the trial including the collection of research MRIs at baseline and 1 year post-op for 80 patients..